In this essay, Zoë Brammer asks whether AI could improve how we diagnose endometriosis and other gynaecological conditions. The essay draws on insights from an interview with Raphaelle Taub – co-founder of Matricis.ai, a startup using AI to democratise MRI expert care for women’s health. Like all the pieces you read here, it is written in a personal capacity.
“Throughout my 20s I sought a diagnosis for increasing debility. Doctors read my notes and wrote me off. When I left off the pill, menstruation became agony; every part of my body seemed to hurt. When I was 27 - a skinny, grey-faced scrap, bleeding continuously and hardly able to stand upright - my disease was named. But it was named on the operating table, and to make me viable I had to lose part of my bladder and my bowel, my womb, and my ovaries. I woke up to a strange future - childlessness, a premature menopause, and a marriage, already tottering, that would soon fall apart.”
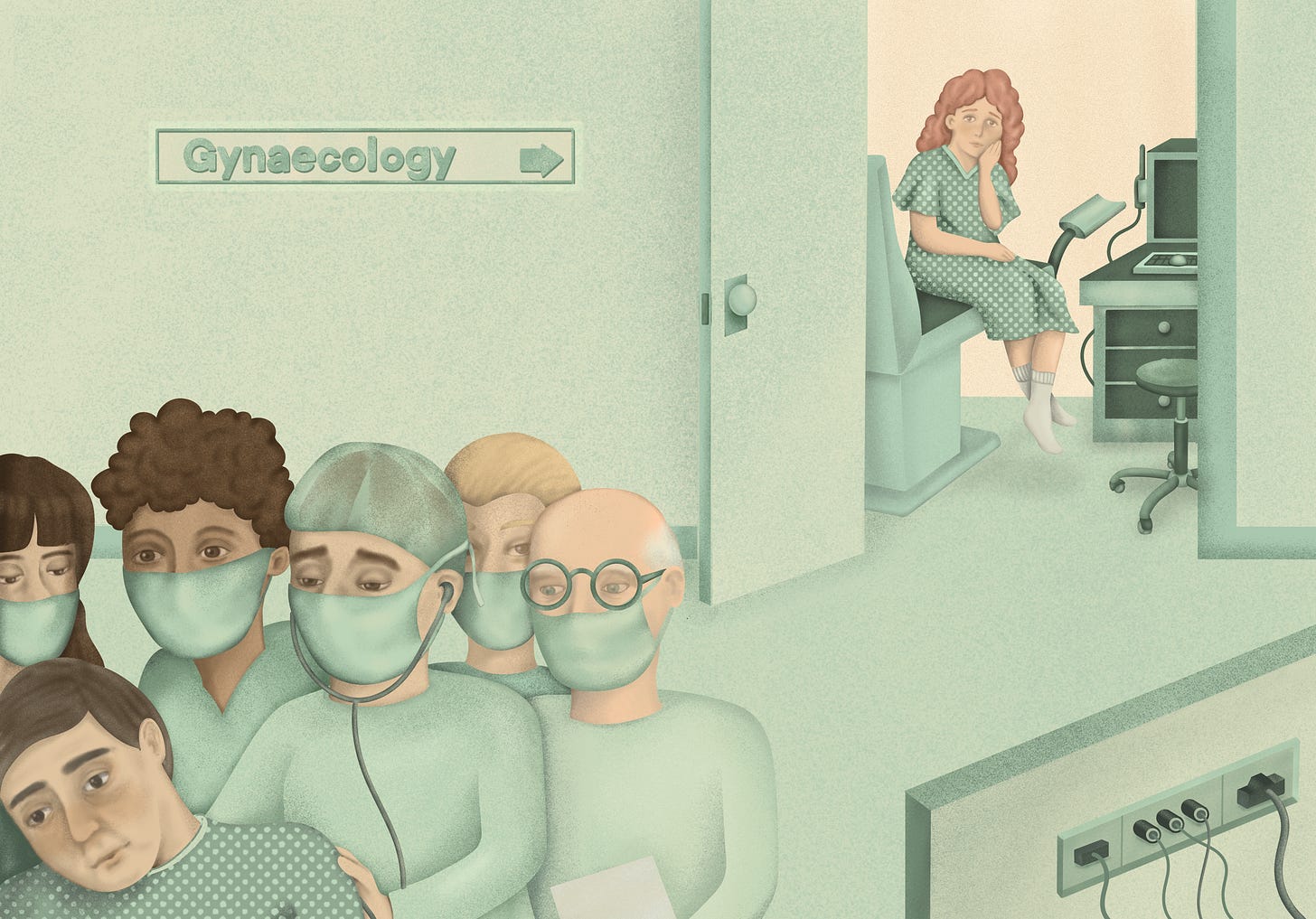
More than 20 years ago, the late author Hilary Mantel documented her experience of being diagnosed with endometriosis - a disease in which tissue resembling the lining of the uterus grows outside it. In extreme cases, this tissue can “bind” other organs together - from the ovaries to the bladder to the bowels - and freeze them in place. ‘Milder’ cases can involve severe pain, heavy menstruation, fertility issues, inflammation, and scar tissue. Current estimates suggest that one in ten women of reproductive age will live with endometriosis, while one in two women will develop a gynaecological condition of some kind — such as fibroids, benign tumours that develop in or around the uterus.
It would be nice to think that diagnostics have gotten better since Mantel’s time, and that AI is now well-placed to accelerate that progress further. However, according to Raphaelle Taub, of the more than 500 AI medical devices approved by the FDA, none are specifically tailored to diagnose gynecological conditions. This absence is also visible in most discussions about AI and healthcare, which tend to centre well-trodden areas like early cancer detection or drug development, while some of the most common and debilitating conditions affecting women remain largely untouched.
The absence of new AI systems for gynaecological health is particularly striking given the lack of existing diagnostic tools and treatments for these conditions. Rates of missed diagnosis remain alarmingly high - up to 60% for endometriosis when MRI scans are used, and as high as 75% with ultrasounds, a more accessible and commonly used option. As Raphaelle notes: “That means that most women who do have the condition are told they don’t, and that erodes trust in the entire medical process.”
A Serendipitous Path
Raphaelle’s entry into this space wasn’t planned. With a PhD in fundamental mechanics and a post-academic pivot into reinsurance, her career was heading in an entirely different direction. That changed when her friend and future co-founder, Élise, shared her own experience of seeking a diagnosis for endometriosis. What began as a personal conversation between friends soon revealed a significant and pressing gap. The problem extended beyond the medical field; it was deeply personal for Élise, for Raphaelle, and for countless women around them — making the silence surrounding these conditions untenable.
Together with their friend Arnaud, who had just completed a post-doc in machine learning, they founded Matricis.ai with the aim of developing diagnostic support tools to help medical specialists more accurately identify these complex conditions. Their goal is to make precise, non-invasive gynaecological diagnosis the norm. But building an AI tool for this purpose involves more than simply applying an off-the-shelf computer vision model to pelvic MRI scans.
To build their tool, Matricis first had to create a dataset of high-quality, annotated pelvic MRI images. As Raphaelle notes: “There are zero open-source annotated MRI datasets of the female pelvis. None. It’s kind of crazy and incredibly annoying.” While some private datasets exist, they’re unlabeled and difficult to access. The technical challenge is compounded by the complexity of pelvic anatomy, which can lead to inconsistencies even among expert annotators. As Raphaelle puts it: “The female pelvis is one of the most complex regions to image. Organs shift, sizes vary. A uterus can range from the size of a palm to that of a watermelon. It’s like doing facial recognition, but the nose might be on your forehead.”
Furthermore, “off-the-shelf models don't work for our task without fine-tuning on labelled data,” Raphaelle told me. “So far, we have found no statistically significant difference in precision, recall, and accuracy metrics between fine-tuning large pre-trained models on our dataset and training a neural network from scratch.” In this context, the choice of base model becomes “a hyperparameter that must be tuned for maximal performance on the application task” — a challenge further complicated by the 3D format of pelvic imaging data, which is not supported by all off-the-shelf large vision models.
Systemic Challenges: Taboo & Neglect
The obstacles are not just technical. Raphaelle was clear: “Women’s health has been overlooked for centuries. It’s still taboo. People don’t talk about their periods or pelvic pain, even with their doctors.” This silence feeds a lack of investment. “There’s so little research that we don’t even agree on prevalence numbers,” she said. “That means pharmaceutical companies can’t estimate market size, so they don’t invest in treatments. And if you don’t have treatments, no one develops diagnostics either. It’s a vicious cycle.”
According to a 2022 survey from Endometriosis UK, 62% of women between the ages of 16-24 don’t know what the condition is - a share that rises to 74% for men (of all ages). This knowledge gap extends to doctors, some of whom fill the gaps with hysteria narratives - speaking of “difficult” women, for whom treatment was not helpful, or who held a perception of their disease that differed from that of their clinician. Today, a non-trivial share of women with endometriosis - and other conditions - are still misdiagnosed with mental health conditions.
These knowledge gaps also reflect a lack of foundational research and practice on gynaecological health. There has long been a pervasive standard in biology and healthcare where women’s bodies are viewed as atypical and men’s bodies as the “norm”. Such inequities affect the problems that are studied, the datasets that are developed, and the experiments that are run. This helps to explain why women have traditionally been underrepresented in clinical trials and why male mice are much more commonly used to test drugs. About 80% of drugs are tested only on male mice, and given that biological sex can play a role in how diseases present, and in how effective or safe drugs and medical devices are, these inequities hurt health outcomes. In 2019, a longitudinal Danish study found that women were diagnosed later than men for many diseases, including an average of two and half years later for cancers, and four and half years later for diabetes.
These trends have compounded and now pose an obstacle to AI being useful in addressing endometriosis and other gynaecological conditions - for example, due to the lack of available data or a shortage of people working on these problems. Positively, women now account for a majority of biology undergraduate students and practising physicians in many countries, following a steady rise in recent decades. However, they remain underrepresented in faculty and senior healthcare roles. They also account for just 22% of AI talent globally. As Raphaelle told me: “At Ecole Polytechnique, the leading engineering school in France, only 16% of students were women in 2024. That imbalance affects the kinds of problems researchers choose to work on. The issue here is not that these challenges are unsolvable, but that they’re often not seen.”
Practical Challenges: Financing & Regulation
For teams working to address these gaps, the path forward is littered with obstacles. First, it remains extremely difficult to get funding to start a women’s health company. Just 2% of healthcare VC funding goes to women’s health startups, while just 1% of global R&D funding targets female-specific conditions (excluding female-specific cancers). With 89% of VC partners being male, and investors demanding "comparables" in a field where few exist, startups like Matricis.ai face an uphill battle for funding — even before a single line of code is written.
This lack of established players and “predicate” devices also makes it harder to navigate the regulatory landscape. In the US, the FDA’s common 510(k) pathway relies on demonstrating substantial equivalence to an existing, legally marketed predicate device. But in nascent fields like AI for gynecology, such predicates can be non-existent. This forces innovators onto more demanding routes, such as the De Novo pathway, which typically requires much more extensive clinical evidence to prove safety and effectiveness from scratch – a significant burden when foundational research and data are already scarce.
Europe presents analogous challenges. The EU's Medical Device Regulation, coupled with new obligations under the EU AI Act, impose rigorous requirements — particularly for novel technologies classified as moderate or high risk, as AI diagnostic tools often are. Compliance involves meticulous documentation through a Quality Management System and assessment by independent "Notified Bodies," or third-party organisations authorised to assess medical devices. While critical for safety, Raphaelle finds that the European emphasis on process — as embodied in the QMS — can feel disproportionate in a field urgently in need of validated outcomes. "The clinical trial is, to me, the biggest safeguard," she says, arguing that the focus should be squarely on proving the technology works through robust trials comparing AI tools to existing diagnostic methods. The extensive documentation and auditing required by these regulations — before large-scale clinical validation might even be feasible for a startup — consumes precious resources and time.
In addition to medical device regulations, Raphaelle highlighted the added complexities posed by data privacy regulations. Processing sensitive health data requires a specific legal basis under the EU’s General Data Protection Regulation, while French law adds further layers — sometimes requiring authorisation from the French data protection agency, the Commission Nationale Informatique & Libertés — for specific uses of data, especially health data warehousing or research that re-uses existing datasets. Compiling and using pelvic MRI data for AI training requires navigating complex consent requirements and technical safeguards.
Raphaelle also highlights the chilling effect that legal ambiguity can have, citing lawyers' warnings about "potential future de-anonymization risks” that could render currently compliant datasets non-compliant. Under the GDPR, pseudonymized data is still considered personal data if re-identification is ’reasonably likely’ — a threshold that is debated, especially in light of recent technological advances. While truly anonymised data falls outside the GDPR’s scope, achieving this with rich datasets — especially when using medical data — is extremely difficult. "Everybody is so scared to be sued," she notes, emphasising the significant cost and delay incurred by simply trying to understand and comply with regulations governing the use of already hard-won data — costs that disproportionately affect smaller companies and underfunded projects. "I understand the idealism," Raphaelle concedes, "but the consequence is that we delay or even block tools that could dramatically improve patients’ lives."
Despite these challenges, Raphaelle remains optimistic that progress is still possible — as long as attention and investment can be directed toward the right problems.
Beyond the Hype: Focus on Untapped Potential
With the right data, investment, and increased awareness, Raphaelle believes the field can overcome decades of neglect. Reliable, non-invasive diagnosis would reduce the need for unnecessary surgeries, restore trust in medical imaging, and accelerate research and drug development by providing a clearer understanding of these conditions. This, in turn, would help address and develop our nearly-nonexistent scientific understanding of these pervasive gynaecological conditions - building awareness and trust. “Good diagnosis is the foundation for everything,” she asserted. “And currently, we’re not even providing women with that.”
When asked what’s over-hyped in AI, Raphaelle didn’t hesitate. “What I find somewhat overhyped in AI today is the focus on technology for its own sake. The capability of modern LLMs are genuinely remarkable, but the conversation often centres on what models can do, rather than on what meaningful problems they could help solve. It sometimes feels like we’re optimising endlessly on benchmarks, while many impactful real-world applications remain overlooked.”
Why Problem Selection Matters More Than Ever
What struck me most wasn’t just Raphaelle’s technical clarity, but her insistence on what’s being left behind. In a field that prides itself on solving hard problems, we have to ask: are we solving the right ones? What happens when the experiences and pain of entire populations are absent from datasets and research labs? The future of AI in healthcare will not be defined solely by the most advanced models; it will be shaped by the choices we make about which problems to address — and for whom we choose to build solutions.




The element of choice is incredibly important and I enjoyed how the piece highlights that! Funding is limited and to what use we put it is everything. I imagine more public education about women's health issues will help re-direct the funds into the right spaces.
In the global south the numbers should be worse, endometriosis just becomes a painful reality that women live with in absence of proper diagnosis and treatment.